Lateral Interbody Fusion (Transpsoas Approach)
Because it involves accessing the spine through a muscle in the side, the lateral interbody fusion offers surgeons and their patients a less-invasive option for spine surgery.
What Is A Lateral Fusion?
Unless you've studied anatomy, chances are you've never heard of the psoas (soh-uhs) muscle. One of the "unsung heroes" of the body, this important muscle extends along the length of the lower spine and is responsible for stability, flexion and range of motion in the lower back and hips.
Precisely because of its size and location, it's also an integral part of a minimally invasive spinal fusion procedure, called lateral interbody fusion, that's been gaining favor in the spine community in recent years.
The direct lateral approach to spinal fusion allows access to the area of the spine to be treated while potentially minimizing disruption of the surrounding soft tissues, nerves and blood vessels.
Gaining clear access to the spine, for both visualization and treatment of the affected vertebrae, is one of the most critical aspects of spinal fusion surgery, and there are several different approaches a surgeon typically takes for an interbody-type procedure. Factors that influence a surgeon's decision on which approach to take include the spinal condition to be treated, its location in the spinal column, his or her own training and surgical experience, available technology and the patient's overall general health.
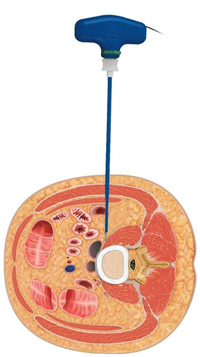
The lateral fusion is different from other interbody fusion techniques in that to approach the spine, the surgeon makes a very small incision in the skin of the patient's side. Then, using minimally invasive surgical techniques, he or she creates a narrow passageway through the underlying soft tissues and the psoas muscle, from the outside of the muscle to the inside gently separating and weaving through the fibers of the psoas muscle rather than cutting through it directly to the vertebra(e) and disc to be treated. This is called the transpsoas, or direct-lateral, approach to interbody spinal fusion, because it involves entering the body for access to the spine through the psoas muscle and soft tissues of the side rather than through the abdominal cavity or through a longer incision in the back.
Why Do I Need This Procedure?
Consisting of the five vertebrae (L1-L5) of the lower back, the lumbar spine bears the greatest amount of the body's weight, making it a common source of back pain. Degenerative conditions, deformity and injury can lead to spinal instability which, if it results in pressure on the spinal cord and/or surrounding nerves, may ultimately cause back pain and/or numbness and muscle weakness that extends into the hips, buttocks and legs.
If these symptoms persist for an extended period of time and have failed to respond to conservative treatment measures such as rest, medication, exercise and physical therapy, your surgeon may recommend a surgical procedure called spinal fusion.
The goal of spinal fusion is to restore spinal stability, and the procedure typically involves removing damaged disc or bone material from in between two adjacent vertebrae (decompression) and then placing bone graft material into the disc space to promote bone growth that permanently joins together the two vertebrae (fusion). Instrumentation such as rods, plates and screws also may be attached to the vertebrae to create an "internal cast" that supports the vertebral structure during the healing process.
How Is A Lateral Fusion Performed?
For a minimally invasive lateral fusion procedure, the patient is positioned on their side on the operating table this is called the lateral decubitus position and sedated under general anesthesia. The surgeon then:
- Using a fluoroscope, a type of moving x-ray machine used in the operating room, ensures proper positioning of the vertebra to be treated.
- Makes a very small incision in the skin in the patient's side, over the midsection of the disc for a single-level fusion or over the intervening vertebral body for a multilevel fusion.
- Using fluoroscopic guidance, inserts a series of dilators through the soft tissues and fibers of the psoas muscle to create a tiny "tunnel" through which the surgeon may view the spine and perform surgery. (A neuromonitoring device also may be used to identify the location of and protect spinal nerve roots.)
Through this narrow opening, your surgeon:
- Removes all or part of the affected disc and surrounding tissues (discectomy).
- Prepares the bone surfaces of the adjacent vertebrae for fusion.
- Inserts bone graft into the disc space to promote fusion.
- Attaches instrumentation, if needed, to the vertebrae for support during the healing process.
- Removes the dilating tubes and closes the incision.
How Long Will It Take Me To Recover?
Your surgeon will have a specific postoperative recovery/exercise plan to help you return to your normal activity level as soon as possible. Following a lateral procedure, you may notice an immediate improvement of some or all of your symptoms; other symptoms may improve more gradually.
The amount of time that you have to stay in the hospital will depend on your treatment plan. You typically will be up and walking in the hospital by the end of the first day after the surgery. Your return to work will depend on how well your body is healing and the type of work/activity level you plan to return to.
Are There Any Potential Risks Or Complications?
All treatment and outcome results are specific to the individual patient. Results may vary. Even though the lateral fusion is minimally invasive, it's important to remember that it is still spine surgery, and therefore not without risk. Complications such as infection, nerve damage, blood clots, blood loss and bowel and bladder problems, along with complications associated with anesthesia, are some of the potential risks of spinal surgery. A potential risk inherent to spinal fusion is failure of the vertebral bone and graft to properly fuse, a condition that may require additional surgery.
It is important that you discuss the potential risks, complications and benefits of direct-lateral interbody fusion with your doctor prior to receiving treatment, and that you rely on your doctor's judgment. Only your doctor can determine whether you are a suitable candidate for this treatment.