Minimally Invasive Lumbar Discectomy
A lumbar discectomy is a spine surgery that involves removing all or part of a diseased or damaged intervertebral disc to relieve pressure on the spinal nerves in the lumbar spine, or lower back. In patients for whom it's appropriate, this procedure may be performed using minimally invasive surgical techniques.
What Is A Minimally Invasive Lumbar Discectomy?
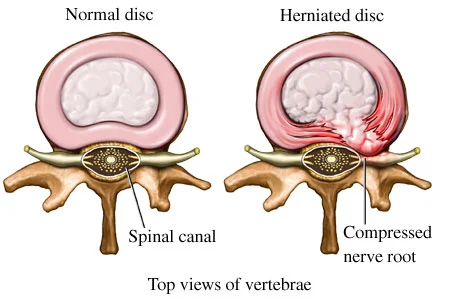
A lumbar discectomy is a surgical procedure that involves relieving the pressure placed on nerve roots and/or the spinal cord by a herniated disc or bone spurs in the lower back – a condition referred to as nerve root compression.
Lumbar refers to the five vertebrae of the lower back. Discs are the spongy, cartilaginous pads between each vertebra, and ectomy means “to take out.” In a lumbar discectomy, the surgeon accesses the lumbar spine through an incision in the back over the vertebral levels to be treated and removes all or part of the disc – and/or in some cases bone material - that’s pressing on the nerves and causing pain. Because it eliminates nerve/nerve root compression, a lumbar discectomy is considered a decompressive spinal procedure.
Depending on your condition and specific surgical goals, your surgeon may choose to perform this procedure using a minimally invasive approach.
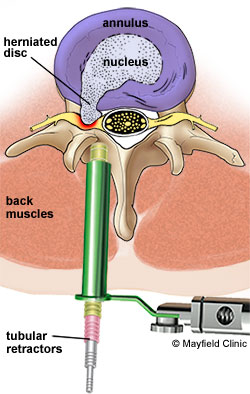
Traditional, open spine surgery involves cutting or stripping the muscles from the spine. Minimally invasive spine surgery involves a small incision or incisions and muscle dilation, allowing the surgeon to separate the muscles surrounding the spine rather than cutting them.
Why Do I Need This Procedure?
A minimally invasive lumbar discectomy may be recommended to relieve pressure placed on the spinal cord or spinal nerves/nerve roots. In general, spine surgery is recommended when intervertebral disc or bone material is pressing into or pinching these neural elements and you are experiencing:
- Leg pain that limits your normal daily activities
- Weakness or numbness in your leg(s) or feet
- Impaired bowel and/or bladder function
How Is A Minimally Invasive Lumbar Discectomy Performed?
The operation is performed with the patient positioned on his or her stomach.
After a small incision is made, the muscles of the spine are dilated, or gently separated, and a tubular retractor is inserted to create a portal through which the surgeon may perform surgery. Through the tubular retractor, a portion of the lamina (the bony vertebral element that covers the posterior portion of the spinal canal) is removed to expose the compressed area of the spinal cord or nerve roots.
Pressure is relieved by removing of the source of compression – all or part of a herniated disc, a rough protrusion of bone called a bone spur, or in some instances a tumor.
The small incision is closed, which typically only leaves behind a minimal scar.
How Long Will It Take Me To Recover?
Your surgeon will have a specific postoperative recovery/exercise plan to help you return to your normal activity level as soon as possible. Following a minimally invasive, you may notice an immediate improvement of some or all of your symptoms; other symptoms may improve more gradually.
The amount of time that you have to stay in the hospital will depend on your treatment plan. In some instances, this procedure may be done on an outpatient basis. You typically will be up and walking in the hospital by the end of the first day after the surgery. Your return to work will depend on how well your body is healing and the type of work/activity level you plan to return to.
Work closely with your spinal surgeon to determine the appropriate recovery protocol for you, and follow his or her instructions as closely as possible to optimize the healing process.
To determine whether you are a candidate for a minimally invasive lumbar discectomy, please talk to your doctor.
Are There Any Potential Risks Or Complications?
All treatment and outcome results are specific to the individual patient. Results may vary. Complications such as infection, nerve damage, blood clots, blood loss and bowel and bladder problems, along with complications associated with anesthesia, are some of the potential risks of spinal surgery. A potential risk inherent to spinal fusion is failure of the vertebral bone and graft to properly fuse, a condition that may require additional surgery.
Please consult your physician for a complete list of indications, warnings, precautions, adverse effects, clinical results and other important medical information that pertains to the minimally invasive lumbar discectomy procedure.